
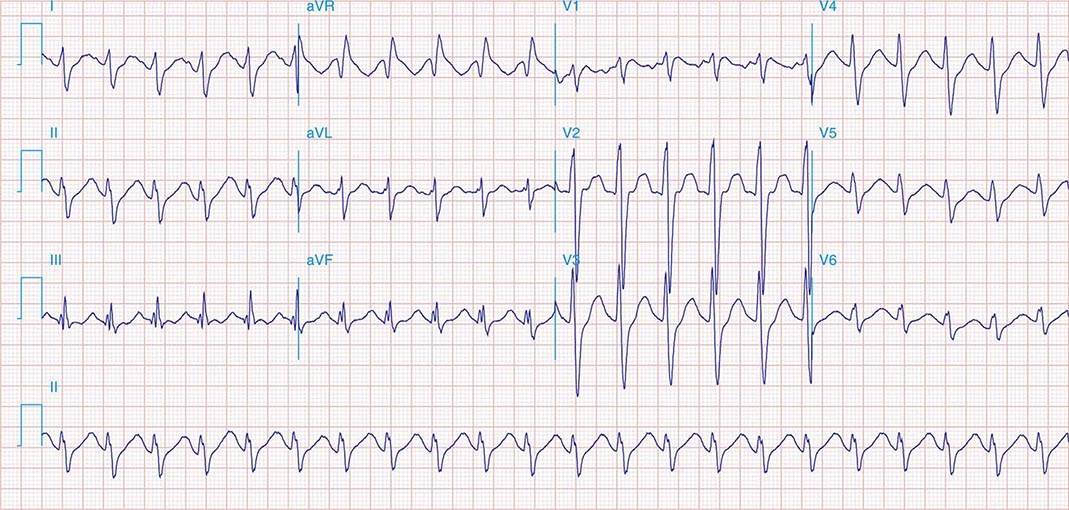
Inverted T waves, like all ST and T wave changes, should always be assessed in the context of the patient presentation, history, and previous ECGs, if available. Acute myocardial infarction can cause left ventricular dysfunction, which can cause backup pressure to the left atrium. The P waves in Lead V1 are biphasic, with the second portion negatively deflected and over 1 mv deep. This is “borderline” for most LAE criteria. The P waves in Lead II are wide (about 10 or 11 ms) and just over 1 mv tall.

In addition to the dramatic T waves, he also has P waves suggestive of “P mitrale”, or left atrial enlargement. Since we know this patient had chest pain, and there is some ST elevation, this should be considered as a cause for his T wave changes. When T waves are deep and symmetrical as they are here, they may be a sign of acute coronary syndrome, or cardiac ischemia. T wave inversions can be secondary to conditions like left ventricular hypertrophy, left bundle branch block, and ventricular rhythms. Some can be due to life-threatening problems like pulmonary embolism, CNS injury, and cardiac ischemia. Some T wave inversions are benign, such as in persistent juvenile T wave pattern. Many conditions can cause inverted T waves, and bedside assessment is necessary to make a certain diagnosis. There are ST segment elevations in Leads V1 and V2. Inverted T waves are present in Leads I, aVL, II, and V3 through V6. This tracing is a good example of widespread, symmetrical inverted T waves. Unfortunately, we don’t have any other clinical information. This ECG is from a 50-year-old man with chest pain. Read more about Left Bundle Branch Block With Left Ventricular Hypertrophy.Since left bundle branch block only occurs in SUPRAVENTRICULAR rhythms, it is important to determine the rhythm, and P waves are a definite sign of SV rhythm. To see the P waves, look at the right chest leads: V1, V2, V3. After a pause, a regular sinus rhythm resumes. The third beat appears to arise from a different focus, which would make it an escape beat, but it is very difficult to determine this due to the very tiny P waves. The first beat appears normal, the second beat is a PAC. It also is easier to diagnose in supraventricular rhythms, because ventricular rhythms usually have large QRS complexes due to the depolarization wave being in one direction across the heart.įor confirmation of LVH, an echocardiogram is recommended. There will be discordant ST segments and T waves, which is called the "strain" pattern. Left ventricular hypertrophy also widens the QRS, although not often as much as LBBB does. The ST segment and T wave will be negative in leads with positive QRS complexes, and positive in leads with negative QRSs (discordant). LBBB is only found in supraventricular rhythms (not ventricular rhythms). The common criteria for left bundle branch block include: wide QRS complex, frontal plane axis normal or leftward, negative QRS in V1, and positive QRS in leads I and V6. For determining LVH by ECG criteria, the Sokolov-Lyon criteria are commonly used ( S wave in V1 + R wave in V5 or V6 > 35 mm). If the ECG criteria for LVH are present, it can be assumed that LVH is present, even in the presence of LBBB. Since the two conditions can have similar ECG changes, it is difficult from the ECG alone to determine the presence of LVH when LBBB is present. The two conditions are very often seen together, in fact, a majority of LBBB patients have LVH. This 92-year-old patient was diagnosed with left bundle branch block on ECG, and left ventricular hypertrophy on echocardiogram.


 0 kommentar(er)
0 kommentar(er)
